RESISTANCE AT A GLANCE

Antimicrobial resistance (sometimes referred to as drug resistance or antibiotic resistance) a natural phenomenon that is due to the mutation and evolution of microorganisms. Today, resistance is one of the most pressing global health issues; causing at least 2 million illnesses and over 20,000 deaths each year. Explore the page below to learn the effects and causes of antimicrobial resistance.
EFFECTS: Why it's dangerous.

Courses of antibiotics before and after surgery have enabled doctors to perform operations that would have been deadly before. Cancer treatments such as chemotherapy and radiotherapy can damage the immune system, but can be boosted with these medications. HIV, HPV, herpes, and hepatitis all require antivirals to alleviate symptoms and prevent spreading. Candidiasis and Sporotrichosis need antifungals to cure. Parasites, such as Malaria, cause over 600,000 deaths worldwide need these medications to combat. The point is, antimicrobials are more widely used than most realize and a world without such medicines would be far more dangerous.
When antimicrobials are ineffective, treatment is hindered, resulting in complications and sometimes even death.
The accessibility of antimicrobials changed the course of history. Numerous diseases previously not treatable can now be cured. However, at the same time the expanding menace resistant microbes threatens the future. Existing medications are now less powerful against previously treatable infections. Illnesses that were effortlessly treatable with mild of antimicrobials now need to be treated with stronger combinations.

When infections become resistant to standard antimicrobials, more expensive drugs must be used. Furthermore, a longer duration of illness and treatment is needed. Thus, increasing health care costs, as well as the economic load on families. According to the Centers for Disease Control and Prevention, antimicrobial resistance in the United States results to an estimated $20 billion a year in excess health care costs, $35 billion in other societal costs and more than 8 million additional days that people spend in the hospital.

COMMON RESISTANT MICROBES
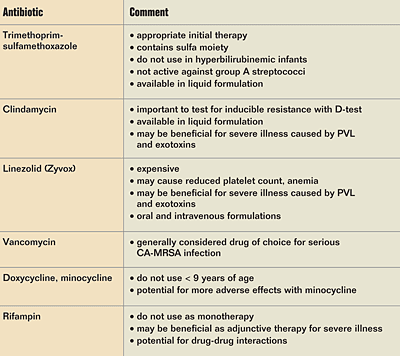
MRSA, Methicillin-Resistant Staphylococcus Aureus, is the leading cause of nosocomial, hospital-acquired, infections in the United States. The reported cost per MRSA patient has ranges between $16,575 and $39,400 in the United States. Approximately 126,000 hospital visits are due to MRSA yearly. 94,000 invasive infections and 19,000 deaths are caused by MRSA yearly as well. One particular strain, CC5, was found was found lacking a set of genes that drive bacteria to kill other bacteria. Additionally, the CC5 strain has a mutation in a gene called dprA, which improves the bacterium's ability to assimilate foreign DNA. Thus, allowing this strain to co-exist with other pathogens and pick up genes that allow further resistance. In fact, the CC5 strain of MRSA has managed to acquire resistance to vancomycin, the last line antibiotic.
BACTERIA:
The two types of resistant tuberculosis are, Multidrug-resistant TB (MDR-TB) and Extensively drug-resistant TB (XDR-TB). MDR-TB is the resistance to two commonly used drugs in the current first-line regimen, isoniazid and rifampin. Outbreaks of MDR-TB are shown to kill 80% of those infected. Treatment requires toxic, second line drugs that are administered over the course of two years and require a six-month period of daily injections. XDR-TB is defined as TB that is resistant to any fluoroquinolone, one of the three second-line drugs (capreomycin, kanamycin, and amikacin), and the two first-line drugs (isoniazid and rifampin). The average cost of treating an individual with TB skyrockets with greater resistance. In 2005, the average cost to treat drug-susceptible TB was $17,000 while $430,000 to treat XDR-TB.

VIRUSES:
Influenza is a diseases that rapidly spreads around the world in seasonal epidemics. Recent estimates show that the cost of influenza epidemics was over $100 million a year in the U.S. Additionally, influenza epidemics result in 3 to 5 million cases of severe illness and over 300,000 deaths annually around the world. In 2006, a combination of influenza and pneumonia accounted for 63, 000 deaths in the United States and was the eighth leading cause of death. Influenza viruses are divided into two groups, influenza A and B. Influenza A has 2 subtypes that affect humans: H3N2 and H1N1. Currently, the H1N1 subtype is associated with the most deaths. These viruses are defined by two different protein components, antigens, that reside on the surface of the virus. They are haemagglutinin and neuraminidase. Today, influenza is treated with neuraminidase inhibitors (oseltamivir, zanamivir, and peramivir) since there is a high level of resistance to the adamantanes class of antivirals.
FUNGI:
PARASITES:



In the United States, the 60 percent of invasive fungal infections are due to Candida (the fungus behind yeast infections). Invasive fungal infections cause a substantial amount of hospitalization and death annually. Each case of Candida bloodstream infection is estimated to result in an additional 3 to 13 days of hospitalization and cost $6,000 to $29,000. Furthermore, some strains of Candida are becoming increasingly resistant to first and second-line antifungal medications, particularly, fluconazole and echinocandins. This creates a problem as the few treatment options remaining are costly and tend to be toxic for patients
Infections with Plasmodium parasites result in Malaria in humans. Among the five species of Plasmodium that infect humans, P. falciparum, the deadliest, causes more than one million malaria-related deaths per year in areas of sub-Saharan Africa, where 90 percent of all malaria-related deaths occur. Recent studies found that nearly 40 percent of the samples it gathered from patients showed resistance to artemisinin, the world's leading antimalarial medication. This drug works by rapidly reducing the main parasite load during the first 3 days of treatment. As of January 2015, artemisinin resistance has been confirmed in Cambodia, the Lao People’s Democratic Republic, Myanmar, Thailand and Viet Nam. Furthermore, there is a substantial risk that multi-drug resistant malaria will develop in this region.
CAUSES: How it happens.

Resistance is fueled by the over-prescribing and misuse of antimicrobial agents.
Since the discovery of penicillin by Alexander Fleming in 1929 (see History), antibiotics, antivirals, antifungals, and antiparastics have flooded the world of medicine. Although beneficial, these drugs have created one of the most urgent global concerns of today's time, as they are often overprescribed by physicians and misused by patients.
Two main types of microbes, bacteria and viruses, are the cause of the majority of infections each year. Antibiotics are what many turn to in the case of one. Although effective against bacteria, antibiotics are more than useless when combating viruses. Nevertheless, millions of prescriptions for antibiotics are written to combat viral diseases, such as Influenza. According to the CDC, antibiotic use could be reduced by over 50 percent without affecting patient health. The reason given by physicians for over prescribing antibiotics is patient demand. Doctors are often are pressured by patients to prescribe antibiotics (along with other antimicrobials), as there are many misconceptions regarding the abilities these drugs. Thus, it is simply easier for physicians, who are pressed for time, to cave and write a prescription for an antibiotic than it is to explain why these drugs may not be the beneficial route.


Even in cases where antibiotics would be effective, few patients take the full course of the medication, thus the pathogen is not completely eliminated. This allows the infection to return with an increased level of resistance since the treatment has only been able to kill off pathogens with low resistance. Therefore, it allows highly resistant bacteria to replicate, spread the resistant gene and return. The returning infection is much worse than the initial one due to the fact that it contains only pathogens with high levels drug resistance. Consequently, a higher dose of antibiotics is needed. By refusing the take the full course of the prescribed treatment, patients play a huge role in drug resistance.

While antimicrobial use in healthcare is a main cause of resistance, its use the agriculture industry is even more prominent. In 2011, 7.7 billion pounds of antibiotics were sold for human consumption to treat illnesses in the U.S. At the same time 29.9 billion pounds were sold for meat and poultry production. Basically, the meat production industry uses 80 percent of the antibiotics produced in the U.S. each year. Some of these antibiotics are given to treat illnesses, but for the most part they given to improve feed efficiency and weight gain in livestock. Because of this, about 12 percent of all retail poultry is infected with salmonella. Additionally, 78 percent of those infections are resistant to at least one antibiotic, while 50 percent is resistant to three or more.